The Role of Trichophytic Closure in Hair Transplant Strip Surgery
In this article, Coalition hair transplant surgeon Dr. William Lindsey provides his expert opinion on the role of trichophytic closure in hair transplantation..
 I have posted lots of topics on hair transplant scar and closure techniques. Indeed, I’ve posted a couple of fairly frank threads on my personal results showing representatives of my own scars ranging from near perfect to poor. The last several years we’ve done roughly 130 hair restoration procedures involving follicular unit strip surgery (FUSS). Based on patient in office followup and pictures that I get emailed to me from travelers, I see about 100 of my own scars at the 2 month scar check and at a year. Out of that number I have seen pretty consistently over at least the last 6 years that I personally get 8 really perfect scars, 4 scars that I’d grade as a C- or D+, and about 88 that are what I’d grade as a B or B+. Now mind you that I am trying to be, but am possibly not totally unbiased. But, I do tell every prospective patient these figures and that sometimes emailed pictures might be better or worse in person. I’m doing the best assessment that I can.
I have posted lots of topics on hair transplant scar and closure techniques. Indeed, I’ve posted a couple of fairly frank threads on my personal results showing representatives of my own scars ranging from near perfect to poor. The last several years we’ve done roughly 130 hair restoration procedures involving follicular unit strip surgery (FUSS). Based on patient in office followup and pictures that I get emailed to me from travelers, I see about 100 of my own scars at the 2 month scar check and at a year. Out of that number I have seen pretty consistently over at least the last 6 years that I personally get 8 really perfect scars, 4 scars that I’d grade as a C- or D+, and about 88 that are what I’d grade as a B or B+. Now mind you that I am trying to be, but am possibly not totally unbiased. But, I do tell every prospective patient these figures and that sometimes emailed pictures might be better or worse in person. I’m doing the best assessment that I can.
I get lots of questions on what a trichophytic closure is, and have posted a bunch of threads on how it was invented to camouflage browlift scars by letting hair behind the forehead cut grow through and in front of the scar so that its harder to detect. Only later on was it “discovered” by hair transplant surgeons and put to excellent use in helping to camouflage strip scars.
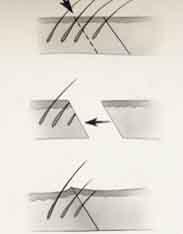
Here is an example of what I’d call a perfect trichophytic closure at the 2 month scar check. It’s a narrow line that still has reddish pigment (normal at 2 months) and clearly growing on both sides of the scar and right through the scar itself, is nice thick hair.

Now there is no way to tell if it will be a perfect scar at 1 year but, on average, a good scar at 2 months will likely be a pretty good or really good scar forever, whereas a poor scar at 2 months will only improve if it’s poor due to shock loss (second case shown, showing scar with left sided shock loss at 2 months, and resolution of this at 6 months).


Lastly, while this is really a great scar, I don’t have any way of predicting who will be the recipient of those 8 poor scars we do each year. The best predictor is how an individual or family member has scarred previously, but still that is an educated guess at best. There is no way to guarantee a perfect scar. We do the best we can to get an excellent scar through pre-op stretching if needed, a limited strip width intra-op-, and a tension-free 2 or 3 layer closure.
Our sutures are removed at day 7 on average and we suggest our patients use vitamin E for 2 months post-op on the scar itself. Despite all that, we still get a few poor scars per year. Just another example of how people are individuals and bring their own physiology to the OR table.
There are no guarantees in medicine, but preoperative discussion of these and other issues, along with research on forums like the Hair Restoration Social Network, allow patients to get as much information as possible prior to making a treatment plan.
Dr. William Lindsey
—-
David (TakingThePlunge)
Editorial Assistant and Forum Co-Moderator for the Hair Transplant Network, the Coalition Hair Loss Learning Center, and the Hair Loss Q & A Blog.
To share ideas with other hair loss sufferers visit the hair loss forum and social community
Technorati Tags: hair transplant, hair restoration, follicular unit strip surgery, FUSS, trichophytic closure



