Information on Trichophytic Closure
Recently, Dr. Ron Shapiro created an extremely informative post on the Hair Restoration Research Forums that addressed and educated forum members on one of the newest innovative techniques in modern hair transplant surgery; the trichophytic closure .
I was recently asked if I perform the “Trichophytic Closure“. The answer is yes. I have been using it routinely since it was presented for the very first time at the annual European Conference in Brussels last summer (6/05).
I‘ve noticed that the level of knowledge and degree of interest about the specifics is fairly high on this forum. So some of you may find it interesting to know more about the history, details, uses and benefits of this technique. If this type of information is useful and appears desired I will continue to do it about other subjects as time goes on. It may be helpful to open up the album I created with photo and diagrams and refer to it as you read:
Photo For Trichophytic Incison Information
TRICHOPHYTIC DONOR CLOSURE
At that annual European Society of Hair Restoration Conference (ESHRS) that took place on 6/05, two physicians (Dr Paul Rose from the USA and Dr Patrick Frechet from France) presented, for the first time, two slightly different variations of this technique. They also referenced and gave credit to a third physician (Dr Mario Marzola from Australia) as having developed a third variation of the technique at around the same time. Dr. Marzola was not present at the European Conference however Dr Marzola did present his variation of the technique at the Annual International Society of Hair Restoration Meeting (ISHRS) it in Australia only a few months later (8/05). These three physicians are each given credit for introducing the technique of the trichophytic closure to the field of hair transplant surgery.
Although relatively new to hair restoration a trichophytic incision is not new to the field of plastic surgery. The idea was actually used in brow lift and other cosmetic surgeries where skin bordered hair in the past. In order to hide a scar created from an incision at the border of the hairline in a brow lift, the initial incision was not made parallel to the hair, but instead, angled the opposite direction (against the grain). This direction of the incision angle transected the follicles and the hope was that these follicles would grow back through and hide the scar. This technique was probably first described by Dr Juri from South America around 1979.
It worked well for brow lifts and flaps and one may wonder why it was not thought of to use during donor harvesting in hair transplantation sooner. If you think about it the answer becomes fairly obvious. One of our primary goals when harvesting donor tissue is to NOT TRANSECT HAIRS. If you transect hairs follicles too far down on the shaft a significant percentage won’t grow or may be lost during the rest of the graft preparation process. The bottom line is that significant transection during donor harvesting can diminishes the patient’s precious and limited supply of donor hair and thereby limits the ultimate amount of coverage and density he can obtain. A lot of practice goes into developing the skill to make the initial donor incisions parallel to the hair in order not to transect them. A skilled practitioner using proper technique can keep his transection rate down to 1-3 percent.
Let’s get back to the trichophytic closure in donor harvesting. As you can see, we cannot make the initial incision when harvesting donor tissue a trichophytic incision that goes against the grain. Too much transection would occur at too deep a level and potentially ruin the donor supply.
However the idea came to a few people in the field (Dr Rose, Dr Frechet, and Dr Marzola) to make the initial incisions parallel to the hair follicles, and then, on one side of the resulting wound, make a second “trichophytic” incision in a very controlled fashion , that trims off a thin strip of epithelium and with it the tips of the hair follicles below. This trimming right below the epithelium is still very high on the hair shaft and does not create any transection that can lead to decreased hair growth. It is controlled transaction very high up on the hair shaft. Then of course the edges are pulled together with the untrimmed side covering the trimmed hairs so the hairs will grow up through and scar and hide it.
DIFFERENCES BETWEEN FRECHET, ROSE AND MARZOLA TRICHOPHYTIC CLOSURES (Figures 1, 2, amd 3 in album)
Photo For Trichophytic Incison Information
There are slight difference between how the above three physicians perform there closure. At this time we do not know whose technique is best ….but all three make an improvement in the appearance of the scar. One of the major differences is that Dr Marzola trims the upper edge of the incision while Dr Frechet and Dr Rose trim the lower edge of the incision.
Although both Dr Rose and Dr Frechet trim the lower edge of the incisions, their respective techniques vary slightly with respect to method that they use to trim away the tissue from the lower edge of the incision. Dr Rose uses a scalpel and first scores the entire length of the incision about 1mm back from the edge. He then uses the scalpel to trims away this 1mm wide piece of tissue just below the epithelium (~1mm deep) so as to only cut off the tip of the hair follicle. It actually looks like he created a ledge or step off with exposed hair shafts hence his name “The ledge technique”
On the other hand Dr Frechet uses a surgical scissor rather than a scalpel to simply trim away the edge of the epithelium from the lower edge. Another difference unique to Dr Frechet is that he also does some minor undermining at the level of the epidermis just below the roots. He feels this further loosen up the skin for a non -tension closure. Dr Rose and Dr Marzola do not feel this undermining is necessary.
The differences between the three trichophytic techniques are minor and all three have helped improve the appearance of donor scars.
ADDITIONAL POINTS RELATED TO THE TRICHOPHTIC CLOSURE
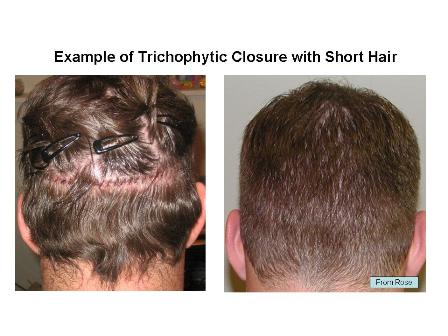
• The primary method a trichophytic closure limits the visibility of a scar is by the camouflage that occurs when hairs grow through the scar. (Figure 4 and 5 in album)
Photo For Trichophytic Incison Information
• A second hypothetical method in which this closure may work is by a postulated “anchoring effect” that may occur. It is theorized that if all the tiny little hairs start growing through the wound edge early they may act as multiple tiny little anchors or “micro sutures” and give extra support to the closure that lasts even after the sutures are removed.
• For scar revisions the use of the trichophytic closure is more variable. It may be effective if the pre-existing scar is thin, there is sufficient laxity remaining, and the entire scar can be excised with limited tension, than it may work well. However if the pre-existing scar is wide and there is decreased laxity than the technique may be less affective for the following reasons. The decreased laxity may make it impossible to remove the entire scar at once. The decreased laxity will increase wound tension and the potential for the new scar to stretch out again. Finally, the edge of wounds in a scar may have less hair present to grow through which limits the effectiveness of the trichophytic closure.
• The Trichophytic closure is not a magic technique that will automatically create a less visible scar if these other rules are not followed. All three innovators of the technique still emphasize that it is still necessary to use all the rules and methods usually employed to create fine scars. (i.e. limit wound tension, create good skin approximation, properly space sutures or staples, etc). As stated above the trichophytic closure does not limit the width of a scar but instead, primarily masks a scar by letting hair grow through it. Since only a 1 to 2 mm wide zone of epithelium is trimmed away, and this creates only a 1-2 mm width of exposed follicles, the trichophytic incision works best when the scar resulting from the donor incision is 1-2 mm or less. When this occurs the results can be amazing and with the scar being nearly undetectable even with the hair cut short. However if the underlying scar resulting from the donor incision is wider than 1-2 mm, for whatever reason, the benefit is less dramatic. There are a number of reasons why a scar may occasionally end up being wider than expected. This is true no matter what technique is used and no matter who the surgeon is.
Figures 6 and 7, in the album show examples of trichophytic closures.
Figures 8 and 9 in the album shows examples of non-trichophytic closures.
Photo For Trichophytic Incison Information
• By far the most common cause of a wider than expected scar is misjudging donor laxity and taking out a strip that causes excess tension on a wound. One reason why the old dogma exists about limiting donor strip size to 1 cm is because it is safe. It is known that nearly 100 percent of patients will not have increased tension if you limit your strip width to 1 cm or less. As you go wider the potential for increased tension and therefore a wider scar goes up. This does not mean you cannot take wider strips, as is obvious by the number of cases being done with wider strips, without significant scarring. But it does mean that you have to use good clinical judgment when deciding who can have wider strips and how wide of a strip is safe. One of the difficulties with trying to predict safe maximum strip widths is the exponential change in tension that begins to occur with very minor increases in width at a certain point (or threshold). To visualize this concept think of a rubber band being stretched. At first you can stretch it quite far very easily but after a certain amount of stretch the tension suddenly increases and goes up dramatically when stretched just a little bit more. Another analogy that may help visualize this concept is that of packing a suitcase. One can put quite a bit of clothes into the suitcase and it will close easily. But then at a certain point (or threshold) even adding one more shirt may prevent it from closing without a struggle.
With harvesting donor tissue it is the same thing ….the donor may close easily at a certain width but at a certain point, when you take out just 1 -2 mm more it may suddenly create a dramatic increase in tension and become hard to close. Dr. Mel Mayer has attempted to develop a testing method for predicting laxity and safe donor widths that he has presented at conferences for the last 3 years. He makes two dots on the donor area about 1 cm apart and pushes the dots together to measures how much they move. Depending on how much the dots move he developed a formula that suggest safe widths ranging from 1-2 cm. So far aside from clinical experience and judgment this is the best we have.
• The ability to predict safe maximum strip widths has become particularly important over the last few years because in order to get the larger sessions that are becoming more popular, a donor strip often has to be greater than 1 cm. It think the old dogma of keeping strip length to 1cm or less in everyone was too conservative. For example, last week I did two cases that were both 4000 + grafts each. I had to make an incision 1.6 cm wide on one and 1.75 cm on the other. But both patients fit my criteria for taking wider strips as they both had tremendous laxity and good donor density. In addition they were both aware of the relative risk (or potential) for a slightly wider scar and they were willing to accept this risk. On the other hand if they had not satisfied my criteria (i.e. – poorer laxity, poor donor density, an increased concern of even a small scar in the donor area, the desire to wear a crew cut, young age with the risk of significant donor hair loss in the future, etc) then I would have suggested a more conservative approach.
Many patients may be candidates for wider donor strips. How wide will vary in different patients. For some it may be too risky to take wider strips while for others it is not. It is important for you as patients to understand the thought process and the criteria physicians use to make these decisions.
The same is true when it comes to other currently controversial aspects of the procedure such as doing larger sessions and higher densities. Larger sessions and higher densities can be done and are powerful tools for us to use in the right candidates. However everyone is not the same and everyone is not a candidate. The criteria we use to decide what to do on different patients needs to be shared and understood.
I know I am beginning to touch on some controversial issues here. I have a lot of thoughts on them and if it is desired I will continue to share them in future posts. For the record I want to state that I am not dogmatic and look at different techniques as tools tool to be added to a physicians armamentarium to be used in the right situations. I think it is important for patients to begin to develop a feel for how different physicians make these types of decisions.
For now when my patient post I will encourage them to give the details of the procedure as well as any criteria I may have used to choose a specific approach. With respect to the donor area I will give them my estimate of donor laxity, donor density, total donor supply as well as the length and width of the strip used. . With respect to the recipient area I will give them the total number of grafts, the total number of hairs, the total breakdown of grafts (1’s, 2’s, and 3’s), the total area transplanted. When referring to densities I will try and be specific about the different densities produced in different areas of the recipient area as the density is not consistent throughout.
Take care,
Ron Shapiro
My Coalition Membership Profile
View highlights from the surgical workshop hosted by Dr. Ron Shapiro
View highlights from the surgical visit to Shapiro Medical Group
Technorati Tags: trichophytic closure