Highlights from the 2014 ISHRS (International Society of Hair Restoration Surgery) Scientific Meeting in Kuala Lumpur, Malaysia
Overview of the 2014 ISHRS Meeting
 Each year, the International Society of Hair Restoration Surgery (ISHRS) holds its annual scientific meeting to discuss hair loss and advancements in medical and surgical hair restoration. This year, the ISHRS meeting was held in Kuala Lumpur, Malaysia and discussion topics focused predominantly on Follicular Unit Extraction (FUE) and future hair loss treatments. This is in stark contrast to past meetings, where FUE was rarely discussed or mentioned as a “novel” or “adjunct” procedure to the then gold standard Follicular Unit Strip Surgery (FUSS).
Each year, the International Society of Hair Restoration Surgery (ISHRS) holds its annual scientific meeting to discuss hair loss and advancements in medical and surgical hair restoration. This year, the ISHRS meeting was held in Kuala Lumpur, Malaysia and discussion topics focused predominantly on Follicular Unit Extraction (FUE) and future hair loss treatments. This is in stark contrast to past meetings, where FUE was rarely discussed or mentioned as a “novel” or “adjunct” procedure to the then gold standard Follicular Unit Strip Surgery (FUSS).
FUE-related presentations included: a discussion of FUE-based Body Hair Transplantation (BHT) from Coalition hair transplant surgeon Dr. Robert True and recommended hair restoration physician Dr. Sanusi Umar; an overview of “treading the FUE path” – or FUE pearls and pitfalls – by recommended physician Dr. Tejinder Bhatti; a presentation on beard hair FUE (a specific type of Body Hair Transplantation) again by Dr. True; a discussion regarding the role of the dull punch in Follicular Unit Extraction given by FUE pioneer and recommended physician Dr. James Harris; a presentation on the challenges of performing FUE in African American patients by Dr. Umar; a discussion about selecting the “right” FUE tool and avoiding graft transection by Coalition physician Dr. Jean Devroye; and an exciting course on the use of manual FUE extraction tools taught by Dr. Jose Lorenzo.
Other interesting presentations included: a talk on designing patient hairlines – featuring Coalition physician Dr. Damkerng Pathomvanich discussing Asian hairline design and Coalition physician Dr. Ron Shapiro discussing Caucasian hairline design; an overview of the most effective graft storage solutions available for hair transplant surgery – featuring a presentation advocating for the use of Hypothermasol by Coalition surgeon Dr. Jerry Cooley and a presentation discussing Plasmalyte from Coalition physician Dr. Timothy Carman; a presentation examining the role of hyaluronidase for taking larger strips with less scarring in FUSS procedures by Dr. True; a presentation on the use of platelet rich plasma (PRP) in hair transplant surgery; and an update on “future” hair loss treatments.
Background on the ISHRS
 The International Society of Hair Restoration Surgery (ISHRS) is the most prominent professional organization for hair restoration in the world. Their primary mission is to educate hair surgeons ranging from the novice to the expert. Their recently renovated website (www.ISHRS.org) provides useful information about hair restoration and profiles and contact information for its 700 plus worldwide physician members. This year’s meeting was conducted by the current ISHRS President Dr. Vincenzo Gambino and program chair Coalition hair transplant surgeon Dr. Damkerng Pathomvanich.
The International Society of Hair Restoration Surgery (ISHRS) is the most prominent professional organization for hair restoration in the world. Their primary mission is to educate hair surgeons ranging from the novice to the expert. Their recently renovated website (www.ISHRS.org) provides useful information about hair restoration and profiles and contact information for its 700 plus worldwide physician members. This year’s meeting was conducted by the current ISHRS President Dr. Vincenzo Gambino and program chair Coalition hair transplant surgeon Dr. Damkerng Pathomvanich.
At the meeting, Coalition member Dr. Sharon Keene replaced Dr. Vincenzo Gambino as the acting President of the ISHRS for the coming year. Congratulations to Dr. Keene for receiving this honor.
Physician Recognition and Awards
Congratulations to the following award recipients:
Recommended hair transplant surgeon Dr. James Harris was awarded the Golden Follicle Award for his role in developing innovative hair restoration techniques and furthering the advancement of hair restoration.
Dr. Ken Washenik won the coveted Platinum Follicle Award for his outstanding achievements in basic science and clinically-related research in hair pathophysiology and anatomy.
Congratulations as well to Dr. Russell G. Knudsen for winning the coveted Manfred Lucas Award for his many contributions to the advancement of physician and staff education.
This year, the Distinguished Assistant Award went to Lauren “Laurie” Gorham, RN of Dorchester, Massachusetts. Laurie Gorham works for Bosley.
Presentations of Interest to Hair Loss Sufferers
Below are the highlights of exciting presentations from our recommended and Coalition physicians – and other hair loss experts – at the 2014 ISHRS conference:
Hairline Design: the Right Hairline for the Right Patient
 Hairline design is one of the most important aspects of hair transplant surgery. Although there are general “rules” for hairline design based upon distance from the brow and Leonardo DiVinci’s rules of proper facial symmetry, significant variation in shape and design exist between different ethnicities. One important variation to understand in hair transplant surgery is the difference between Asian and Caucasian hairlines. As a renowned expert on hair transplant in individuals of Asian descent, Dr. Damkerng Pathomvanich was asked to explain his approach to Asian hairline design.
Hairline design is one of the most important aspects of hair transplant surgery. Although there are general “rules” for hairline design based upon distance from the brow and Leonardo DiVinci’s rules of proper facial symmetry, significant variation in shape and design exist between different ethnicities. One important variation to understand in hair transplant surgery is the difference between Asian and Caucasian hairlines. As a renowned expert on hair transplant in individuals of Asian descent, Dr. Damkerng Pathomvanich was asked to explain his approach to Asian hairline design.
According to Dr. Pathomvanich, Asians possess unique skull shapes with less forehead projection and different facial features. This requires a “flatter” more “U-shaped” hairline design. Many hair restoration physicians don’t realize this, and drawing a traditional Caucasian hairline on an Asian patient often results in poor facial framing.
 Dr. Ron Shapiro, on the other hand, is an expert on Caucasian hairline design. Dr. Shapiro was one of the first physicians to truly appreciate and demonstrate the benefit of macro and micro irregularity in Caucasian hairline design; he also understands the importance of designing hairlines with future hair loss in mind, and shared both these principles in his presentation. Together, Dr. Pathomvanich and Dr. Shapiro’s presentations demonstrated the importance of designing the “right hairline for the right patient.”
Dr. Ron Shapiro, on the other hand, is an expert on Caucasian hairline design. Dr. Shapiro was one of the first physicians to truly appreciate and demonstrate the benefit of macro and micro irregularity in Caucasian hairline design; he also understands the importance of designing hairlines with future hair loss in mind, and shared both these principles in his presentation. Together, Dr. Pathomvanich and Dr. Shapiro’s presentations demonstrated the importance of designing the “right hairline for the right patient.”
Graft Storage Mediums: Best Way to Store Grafts During Hair Transplant Surgery?
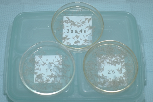 Graft storage is a crucial aspect of hair transplant surgery. In fact, inappropriate storage of extracted follicular unit grafts can lead to desiccation (“drying out”) and poor growth after implantation. So, how should physicians store grafts during hair transplant procedures?
Graft storage is a crucial aspect of hair transplant surgery. In fact, inappropriate storage of extracted follicular unit grafts can lead to desiccation (“drying out”) and poor growth after implantation. So, how should physicians store grafts during hair transplant procedures?
 According to Coalition hair transplant surgeon Dr. Timothy Carman, a complicated solution historically hasn’t always been utilized; Plasmalyte A – a simple solution containing water, sugar, sodium, potassium, and magnesium – has been used with great success over the years. While new, “advanced” products exist, such as those used in his practice, Dr. Carman reviewed how Plasmalyte A has stood the test of time and as an effective graft storage medium.
According to Coalition hair transplant surgeon Dr. Timothy Carman, a complicated solution historically hasn’t always been utilized; Plasmalyte A – a simple solution containing water, sugar, sodium, potassium, and magnesium – has been used with great success over the years. While new, “advanced” products exist, such as those used in his practice, Dr. Carman reviewed how Plasmalyte A has stood the test of time and as an effective graft storage medium.
 Coalition hair transplant surgeon Dr. Jerry Cooley reviewed Hypothermasol – a new storage medium that eliminates free radicals, provides pH balance, features several energy substrates (ATP), and promotes a balanced ionic concentration, which may offer superior graft storage. According to Dr. Cooley, Hypothermasol reduces cell death, improves follicle survival, creates better post-implantation yields, and leads to better results. So, which storage medium is best? It’s difficult to say. Each has merit and, much like surgical tools and techniques, each surgeon has their own preference. It’s important that patients discuss graft storage mediums with physicians and understand exactly how their grafts will be stored on the day of surgery.
Coalition hair transplant surgeon Dr. Jerry Cooley reviewed Hypothermasol – a new storage medium that eliminates free radicals, provides pH balance, features several energy substrates (ATP), and promotes a balanced ionic concentration, which may offer superior graft storage. According to Dr. Cooley, Hypothermasol reduces cell death, improves follicle survival, creates better post-implantation yields, and leads to better results. So, which storage medium is best? It’s difficult to say. Each has merit and, much like surgical tools and techniques, each surgeon has their own preference. It’s important that patients discuss graft storage mediums with physicians and understand exactly how their grafts will be stored on the day of surgery.
Role of Body Hair Transplants (BHT) in Modern Hair Restoration Surgery?
 According to Coalition hair transplant surgeon Dr. Robert True, Body Hair Transplants (BHT) play an important role in modern hair restoration surgery. Dr. True admits that scalp follicles are the best source of grafts for hair transplant procedures. He understands this is not always an option, however, and occasionally patients need to utilize other reserves – like grafts from the beard and torso. Dr. True believes body hair grafts with hair characteristics most similar in length, texture, and behavior to scalp follicles are beneficial for patients with depleted scalp donor supply who need additional surgery. These grafts, according to Dr. True, are very delicate and must be extracted carefully and only stored for a minimal amount of time before implantation. Otherwise, they will desiccate (dry out) and become traumatized during handling and insertion.
According to Coalition hair transplant surgeon Dr. Robert True, Body Hair Transplants (BHT) play an important role in modern hair restoration surgery. Dr. True admits that scalp follicles are the best source of grafts for hair transplant procedures. He understands this is not always an option, however, and occasionally patients need to utilize other reserves – like grafts from the beard and torso. Dr. True believes body hair grafts with hair characteristics most similar in length, texture, and behavior to scalp follicles are beneficial for patients with depleted scalp donor supply who need additional surgery. These grafts, according to Dr. True, are very delicate and must be extracted carefully and only stored for a minimal amount of time before implantation. Otherwise, they will desiccate (dry out) and become traumatized during handling and insertion.
Recommended physician Dr. Sanusi Umar – a body hair transplant pioneer – agrees, and frequently tries to improve the use of body hair transplants in new and innovative ways. One of his new discovers involves a novel approach to eyelash restoration: using leg hair follicular unit grafts for eyelash transplant surgery. Dr. Umar noted that the naturally short and curled leg hair follicles mimic eyelash hair, and concluded that leg hair follicles could be useful in eyelash transplantation.
He tested his theory by comparing two patients: one who underwent eyelash transplantation with scalp follicles and another who underwent surgery with leg hair follicles. After 3 months, both patients had a yield of 80-85%. The scalp follicle patient required eyelash trimming every 2 weeks and used mascara and curlers to shape the lashes. The leg hair patient, on the other hand, required no trimming and noted effective shape and curl in the transplanted lashes without the use of mascara and curling tools. Dr. Umar believes eyelash transplantation with leg hair follicles may represent a new use of body hair transplants.
To review the results of this case, please see the following: FUE Eyelash Transplant with Leg Hair.
Role of the Dull Punch in FUE
 Recommended hair transplant surgeon Dr. James Harris is an FUE pioneer. As the inventor of both the manual SAFE FUE dull punch and the motorized SAFE system, Dr. Harris revolutionized the role of the “dull” punch in Follicular Unit Extraction.
Recommended hair transplant surgeon Dr. James Harris is an FUE pioneer. As the inventor of both the manual SAFE FUE dull punch and the motorized SAFE system, Dr. Harris revolutionized the role of the “dull” punch in Follicular Unit Extraction.
 According to Dr. Harris, dull punch graft extraction is still extremely effective. Dull punch extraction allows for a deeper dissection – up to 4mm, which creates less extraction force and boasts transection rates as low as 2.8%. Blunt extraction is an effective technique in the right hands, and Dr. Harris believes it still has an important role in FUE.
According to Dr. Harris, dull punch graft extraction is still extremely effective. Dull punch extraction allows for a deeper dissection – up to 4mm, which creates less extraction force and boasts transection rates as low as 2.8%. Blunt extraction is an effective technique in the right hands, and Dr. Harris believes it still has an important role in FUE.
Hyaluronidase in Follicular Unit Strip Surgery (FUSS): a Safe Way to Take Large Strips with Less Scarring?
 Hyaluronidase (HRH) is a natural enzyme that breaks down the body’s intracellular matrix (the connective tissue between cells) and is frequently utilized in cosmetic procedures. In 2013, Coalition hair transplant surgeon Dr. Jerry Cooley started using hyaluronidase for another purpose: creating scalp laxity for larger strip extractions without increased scarring in Follicular Unit Strip Surgery.
Hyaluronidase (HRH) is a natural enzyme that breaks down the body’s intracellular matrix (the connective tissue between cells) and is frequently utilized in cosmetic procedures. In 2013, Coalition hair transplant surgeon Dr. Jerry Cooley started using hyaluronidase for another purpose: creating scalp laxity for larger strip extractions without increased scarring in Follicular Unit Strip Surgery.
After being introduced to the technique by Dr. Cooley, Dr. Robert True began using hyaluronidase in his practice. Dr. True routinely began injecting the donor regions of patients with hyaluronidase before strip extraction. He used this technique in three specific patient populations: individuals seeking the largest strip harvest possible; patients with a previous donor scar; and patients with inelastic scalps. Dr. True has injected over 150 patients with hyaluronidase before strip extraction. After reviewing the results, Dr. True observed the following: hyaluronidase typically increased strip harvest by 20-50%; despite increased strip widths, the resulting donor scars were typically 1mm (+/-) wide; and while less than 5% of patients noted increased temporary shedding in the donor region, no long-term complications were revealed. From this, Dr. True concluded that using hyaluronidase in strip procedures is an effective way of increasing strip width and maximizing harvest without creating wider donor scars.
Future Hair Loss Treatments: Is Bimatoprost (Latisse) the Next Treatment for Androgenic Alopecia (AGA)?
 “Future” hair loss treatments remained a popular topic at this year’s ISHRS conference. The biggest “buzz” focused around the use of bimatoprost or “Latisse” as a new, non-surgical hair loss treatment. Originally tested as a glaucoma drug, bimatoprost was found to increase the density, length, and darkness of eyelashes. Several years later, the drug was approved by the FDA for thin eyelashes under the brand name “Latisse.” During this same time period, hair loss researchers made an interesting discovery: prostaglandins – fatty compounds that play hormone-like roles in the body – play an important role in hair follicle regulation. For example, researchers found that prostaglandin D2 (PGD2) creates follicle miniaturization and plays a role in androgenic alopecia (AGA); while prostaglandin F2 (PGF2) stimulates follicle growth. Knowing that bimatoprost is a prostaglandin F2 analog and stimulated eyelash growth, the scientific community wondered if it could play a role in androgenic alopecia. Research trials quickly started and showed efficacy in mouse models. This cleared the path for human trials, and bimatoprost is now in phase 2 clinical trials for androgenic alopecia in the US.
“Future” hair loss treatments remained a popular topic at this year’s ISHRS conference. The biggest “buzz” focused around the use of bimatoprost or “Latisse” as a new, non-surgical hair loss treatment. Originally tested as a glaucoma drug, bimatoprost was found to increase the density, length, and darkness of eyelashes. Several years later, the drug was approved by the FDA for thin eyelashes under the brand name “Latisse.” During this same time period, hair loss researchers made an interesting discovery: prostaglandins – fatty compounds that play hormone-like roles in the body – play an important role in hair follicle regulation. For example, researchers found that prostaglandin D2 (PGD2) creates follicle miniaturization and plays a role in androgenic alopecia (AGA); while prostaglandin F2 (PGF2) stimulates follicle growth. Knowing that bimatoprost is a prostaglandin F2 analog and stimulated eyelash growth, the scientific community wondered if it could play a role in androgenic alopecia. Research trials quickly started and showed efficacy in mouse models. This cleared the path for human trials, and bimatoprost is now in phase 2 clinical trials for androgenic alopecia in the US.
Treading the FUE Path: Pearls and Pitfalls: Dr. Tejinder Bhatti
Introduction
Those who have followed the development and evolution of hair transplantation tools and techniques over the past few years know that follicular unit extraction (FUE) is becoming increasingly popular among hair loss sufferers seeking surgical hair restoration. This is due, in part, to the fact that FUE is less invasive than follicular unit strip surgery (FUSS) and the lack of a linear strip scar offers the potential to wear a close cropped haircut. However, the real catalyst for this recent explosion of interest in the procedure may be that FUE practitioners have worked diligently to increase the efficacy of the procedure. Today’s FUE sessions can exceed 2,000 grafts in a single day when appropriate for the patient, with a high rate of success; a feat unheard of only a few short years ago.
 One such dedicated FUE surgeon is recommended hair restoration physician Dr. Tejinder Bhatti of Chandigarh, India. Since dedicating his clinic to full time FUE, Dr. Bhatti has become a leading expert on FUE and body hair transplantation (BHT). In this presentation, Dr. Bhatti highlights “possible disastrous outcomes”, addresses “concerns about safe FUE technique” and discusses the causes and developments of disastrous results while suggesting tips to avoid them.
One such dedicated FUE surgeon is recommended hair restoration physician Dr. Tejinder Bhatti of Chandigarh, India. Since dedicating his clinic to full time FUE, Dr. Bhatti has become a leading expert on FUE and body hair transplantation (BHT). In this presentation, Dr. Bhatti highlights “possible disastrous outcomes”, addresses “concerns about safe FUE technique” and discusses the causes and developments of disastrous results while suggesting tips to avoid them.
Substantiating Data:
This presentation is the result of my 3 year experience of 1518 cases of FUE since September, 2010 when we at the clinic made the complete transition from follicular unit strip surgery (FUSS) to FUE after realizing the safety, effectiveness and patient friendliness of the technique. We use blunt Harris punches which may vary in diameter from 0.65-0.85mm in diameter. Only mechanical (motorized) extraction is done using the Safe Scribe system of Dr. James Harris. The peer certified rate of extraction varies from 1200 to 2000 per hour (average 1400). As we have trained over 220 doctors from India and abroad in FUE technique, our technique stands peer reviewed and so do the facts we reveal.
Discussion:
Bad results or disasters ensue after a hair transplant due to one or more of the following reasons:
- Over-harvesting – Whenever more than 20% of the donor hair are harvested, there is excessive “show “of the donor area after unharvested hair regrows.

- Angulation of slits – This 32-year-old patient received wrong angulation of slits. The slits for the hairline have been made at 70-90 degrees. The temple slits have been also made in the wrong direction and more so the natural curl of hair has been ignored. This gives a disastrous look to hide which the patient keeps his hair cropped close. Another bad technique as seen is the placement of grafts with 2-3 follicles in the leading temple row. The condition was revised by extracting the mal-positioned grafts and placing them in normal angulation. More grafts were harvested to increase the low density.
- Suboptimal growth – Poor growth but marked scarring resulting from prolonged graft out of body time. The neophyte surgeon single handedly harvested 2300 grafts, planted half the same day over 9 hours himself and the remaining the next morning. This case exemplifies the benefits of teamwork.
- Improper technique – The first patient below underwent a procedure in another town and called up seeking help for bleeding both from donor and recipient areas at night. The pictures were e-mailed the same night. The surgeon has crossed the boundaries of the defined safe zone, has traumatically over-harvested in all areas, has used a large diameter punch and caused a high transection rate. This case reflects all that points of poor surgical technique.
These 3 cases were done in 2011 using FUE technique with large diameter punches of size 2 mm resulting in a classic doll’s head look, pitting of grafts, low density and an overall unaesthetic look.
- Scarring – The photo below shows one of the worst strip scars. If well done, FUSS leaves barely discernible scars.
Visible scars with sequestration cyst formation. Scars due to use of 2 mm punches, which are very much in use today, under the garb of FUE. Cysts form due to improper inspection for buried grafts at the end of the harvesting.
Large punch size resulting in prominent scarring in the donor area.
- Transgressing the “safe” zone – The surgeon has gone into the safe zone to harvest. The picture is 18 months after the procedure and receded hairline now reveals marks of FUE extraction. Needless to say that grafts taken from this area would have lived a short lifespan.
Malpractice – “100 free grafts Trial”- This patient is a victim of an aggressive “promotional offer”. The grafts have been placed in such a strategic position that the patient has
The posterior hairline has been deliberately formed in a straight line to make it look artificial so he returns for the next procedure sooner than 6 months.
Conclusion:
If you believe that FUE is the oldest surgical hair restoration procedure, we have come full circle. Gone is the era that associated punch grafting with bad pluggy, doll-head results. Today’s FUE is a refined procedure that utilizes miniscule punches which range in size from 0.65- 0.85 mm to provide an undetectable, natural result with high density without leaving a visible linear scar. As a prominent FUE learning center in Asia, Dr. Bhatti in India realized and projected 3 years ago the force of FUE, its wide acceptance being minimally invasive in nature, and the value it brings to the field of surgical hair restoration. Having trained over 190 doctors in the past 3 years alone, he never came across a doctor who would have liked to learn strip as well after seeing the potential of the procedure to harvest a large number of grafts in a single session. The decline of strip is mostly related to the linear scar which gets broader and therefore more visible after each repeat session. No amount of trichophytic closure or w-plasty can make it invisible when sporting no.1 or 2 size hair. It was a conscious decision to switch over to FUE keeping in mind the increasing demand of the procedure in India amongst a population which is wary of surgical techniques for cosmesis. However, Dr. Bhatti continues to offer the strip method to patients with-
- Female pattern baldness
- Type VI Male pattern baldness- to enhance the yield from scalp hair
It has been Dr. Bhatti’s experience that even this miniscule subset of patients would rather have grafts harvested from their beard, chest, etc. rather than live with a visible linear scar all their lives.
FUE in African American Hair: Dr. Sanusi Umar
 Recommended hair transplant surgeon Dr. Sanusi Umar of Redondo Beach, CA demonstrated a new tool and FUE approach that is successful in doing all Afro-textured hair, regardless of hair kinkiness or tissue characteristics. It is a patent pending, non-rotary FUE punch that can work manually or be mounted on an ultrasonic hub.
Recommended hair transplant surgeon Dr. Sanusi Umar of Redondo Beach, CA demonstrated a new tool and FUE approach that is successful in doing all Afro-textured hair, regardless of hair kinkiness or tissue characteristics. It is a patent pending, non-rotary FUE punch that can work manually or be mounted on an ultrasonic hub.
Normally, with a great deal of difficulty, conventional FUE punches would be successful in 10-30% of patients with afro-textured hair. Dr. Umar has worked for over 6 years developing a device and method that can successfully tackle even the kinkiest hair and he succeeded with this tool,which also has a version for patients with straight hair and loose wavy hair as well.
Patients Presented
Case 1: A patient who had recorded over 60% transection with all conventional methods of FUE including several test procedures at Dr. Umar’s clinic. He was seen by another physician in Beverly Hills who presented as having FUE success in this demographic. Unfortunately, his yield was very poor and now had significant FUE scarring in the head donor area that increased the difficulty level of any future FUE procedure. The new tool and method presented at the 2014 meeting in Kuala Lumpur was highly successful with a transection rate of less than 10%.
Case 2: FUE test using Dr. Umar’s existing rotary punches showed transection rates of over 50%. The new tool and method performed with a transection rate of less than 5%
Conclusion
Unfortunately, the details presented at this year’s ISHRS meeting are currently classified pending publication of the work in a scientific peer-reviewed-journal. There are also proprietary matters as well as data collection expected to be completed before January 2015. These tools should be made available at the next ISHRS meeting in Chicago to interested FUE practitioners. Dr Umar has already proposed (to the next meeting chair) a live workshop to teach methods of use to attendees at the 2015 meeting.
ARTAS: Robotic Recipient Site Creation: Dr. Robert Bernstein
 Dr. Robert Bernstein is an esteemed member of the Coalition of Independent Hair Restoration Physicians. He is also Clinical Professor of Dermatology at the College of Physicians and Surgeons of Columbia University in New York and is one of the first hair transplant surgeons to introduce robotic FUE into his practice. Dr. Bernstein has been involved in the research and development of robotic FUE and robotic recipient site creation.
Dr. Robert Bernstein is an esteemed member of the Coalition of Independent Hair Restoration Physicians. He is also Clinical Professor of Dermatology at the College of Physicians and Surgeons of Columbia University in New York and is one of the first hair transplant surgeons to introduce robotic FUE into his practice. Dr. Bernstein has been involved in the research and development of robotic FUE and robotic recipient site creation.
Introduction
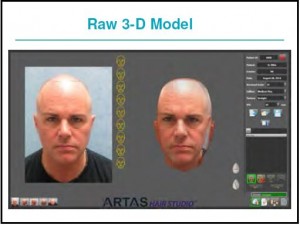
The first robot to assist in follicular unit transplant procedures was released in the fall of 2011. The initial application was the in-vivo separation of follicular units from the surrounding scalp tissue. With new hardware and software capabilities, the robot can now create recipient sites. Preliminary observation suggests that it can perform this function with greater precision and consistency than can generally be accomplished manually.
Method
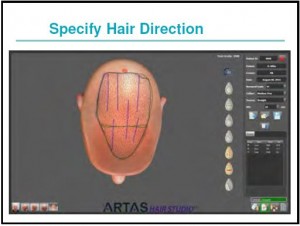
For robotic recipient site creation, the doctor first draws a hairline and other markings directly onto the patient’s scalp to delineate the area to be transplanted. Next, multiple photographs are taken of the patient and software converts the images and markings into a 3-D model of the patient.
The physician then specifies the angle of hair elevation and direction, average density, total number of the recipient site incisions and recipient site depth. The robotic device uses image-guided technology to avoid hairs of a specific diameter. In this way, the new distribution of sites can be made to complement the distribution of existing terminal hairs (or the hair from prior hair transplant procedures), while at the same time ignoring hair that is miniaturized or vellus.
The imaging software for site creation can be used as an integrated system for both designing the restoration at the consult and guiding the surgery. It also can be used independently as a consulting tool, or in the OR guiding the creation of recipient sites.
Conclusion
In performing recipient site creation, the robot automates another part of the hair transplant process that can be prone to human variability and error. The new technology also gives the physician a tool at the time of the consult to show what the hair restoration procedure can do and to better align the patient’s expectations with anticipated results.
Low Level Laser Therapy (LLLT): How Does it Work? What is the Difference Between the Different Devices?
 Low-level laser treatment for hair growth remains one of the most hotly debated hair loss treatments. At this year’s meeting, Coalition hair restoration physician Dr. Sharon Keene of Tucson, AZ presented the results of her LLLT research which yielded important information that consumers considering purchasing a laser device should know.
Low-level laser treatment for hair growth remains one of the most hotly debated hair loss treatments. At this year’s meeting, Coalition hair restoration physician Dr. Sharon Keene of Tucson, AZ presented the results of her LLLT research which yielded important information that consumers considering purchasing a laser device should know.
Dr. Keene has found that beaming laser or any other light on to hair seems unlikely to get to scalp. Only very thin hairs will allow the light to penetrate if the scalp is exposed properly. If light is not perpendicular to the scalp or not touching the scalp, it is likely not to work well or at all. This means that laser hoods and overhead devices cannot make the same claims that devices such as the HairMax LaserComb that touch the scalp do. Also, there are fundamental flaws in recent LLLT studies. Their hair counting methods appeared to be inaccurate so results are not reliable (except the laser comb–but results were modest and no one knows if they are sustainable).
Meeting Conclusion
The fields of medical and surgical hair restoration continue to develop and improve thanks to the efforts of skilled and experienced hair restoration physicians like those recommended on The Hair Transplant Network.
We would like to extend our thanks to those physicians who attended this year’s ISHRS meeting in San Francisco and contributed to the writing of this presentation.
Technorati Tags: 2014 ISHRS Meeting, International Society of Hair Restoration Surgery, ISHRS, hair loss, hair restoration, Follicular Unit Extraction, FUE, future hair loss treatments, Follicular Unit Strip Surgery, FUSS, hair transplant, Asian hairline design, Caucasian hairline design, graft storage solutions, hair transplant surgery, platelet rich plasma, PRP, Dr. Damkerng Pathomvanich, Dr. Ron Shapiro, Dr. Timothy Carman, Plasmalyte A, Dr. Jerry Cooley, Hypothermasol, graft storage, Body Hair Transplants, BHT, hair restoration surgery, body hair transplant, eyelash restoration, eyelash transplant, Dr. James Harris, SAFE FUE, Hyaluronidase, HRH, bimatoprost, Latisse, PGD2, androgenic alopecia, hair transplantation, Dr. Tejinder Bhatti, Dr. Sanusi Umar, Dr. Robert Bernstein, Low-level laser treatment, hair growth, hair loss treatments, Dr. Sharon Keene, HairMax LaserComb