Highlights from the 2015 ISHRS (International Society of Hair Restoration Surgery) Scientific Meeting in Chicago
 Overview of the 2015 ISHRS Meeting
Overview of the 2015 ISHRS Meeting
The International Society of Hair Restoration Surgery (ISHRS) held its annual scientific meeting in Chicago, Illinois this year. The yearly gathering brings together many of the world’s leading hair transplant surgeons and hair loss researchers to discuss advancements in medical and surgical hair restoration. Continuing the trend from last year’s meeting, discussion topics focused predominantly on Follicular Unit Extraction (FUE) and future hair loss treatments.
Background on the ISHRS
The International Society of Hair Restoration Surgery (ISHRS) is the most prominent professional organization for hair restoration in the world. Their primary mission is to educate hair surgeons ranging from the novice to the expert. Their website (http://www.ishrs.org/) provides useful information about hair restoration and profiles and contact information for its 700 plus worldwide physician members. This year’s meeting was conducted by the current ISHRS President Coalition hair transplant surgeon Dr. Sharon Keene and program chair Dr. Nilofer Farjo.
At the meeting, Dr. Kuniyoshi Yagyu replaced Dr. Sharon Keene as the acting President of the ISHRS for the coming year. Congratulations to Dr. Yagyu for receiving this high honor.
Physician Recognition and Awards
Congratulations to the following award recipients:
Coalition hair transplant surgeon Dr. Bernard P. Nusbaum was awarded the Golden Follicle Award for his role in developing innovative hair restoration techniques and furthering the advancement of hair restoration.
Dr. Pierre Bouhanna won the coveted Platinum Follicle Award for his outstanding achievements in basic science and clinically-related research in hair pathophysiology and anatomy.
Congratulations as well to Dr. Shoji Okuda for winning the coveted Manfred Lucas Award for his many contributions to the advancement of physician and staff education.
This year, the Distinguished Assistant Award went to Janna E. Shafer. Lead Medical Tech and Surgical Manager for the Shapiro Medical Group.
Presentations of Interest to Hair Loss Sufferers
Below are the highlights of exciting presentations from our recommended and Coalition physicians – and other hair loss experts – at the 2015 ISHRS conference:
Advances in Follicular Unit Extraction (FUE) and How It Compares to FUSS (Strip) Surgery: Is FUE the New ‘Gold’ Standard?
The roots of follicular unit extraction (FUE) hair transplantation stretch back almost 30 years. For most of that time, FUE largely remained a niche procedure reserved for patients with limited balding or for small touch up sessions, while follicular unit strip surgery (FUSS) became the gold standard of surgical hair restoration. However, in recent years FUE has exploded in popularity with some clinics completely abandoning strip and devoting their entire practice to the procedure.
This rise in popularity may be due in part to the mistaken idea among prospective patients that FUE is a “scarless” procedure. Though no surgery is truly scarless, FUE does offer the potential to wear a buzz cut with no visible scarring. Continued advancements in FUE tools and techniques allowing some hair transplant surgeons to perform large sessions exceeding 2,500 grafts in a single day are also factors that have made FUE the procedure of choice for many hair transplant patients.
This has led some hair restoration physicians to examine hair growth success rates between the two procedures in order to determine if FUE is now a viable alternative to strip or still best used as an adjunct in limited cases.
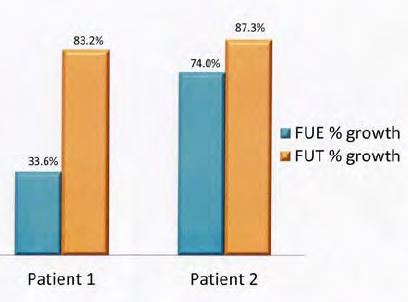
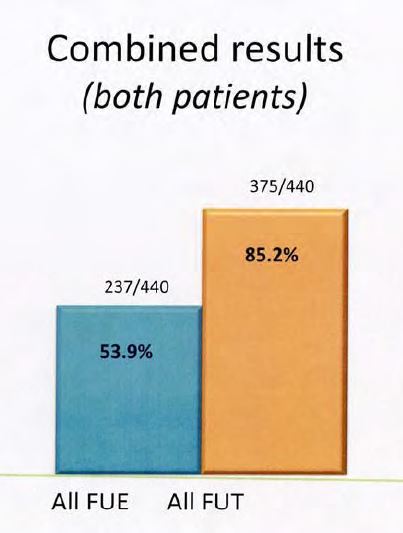
 Coalition hair transplant surgeon Dr. Michael Beehner conducted a comparative study of FUE and FUSS in 4 of his patients. His findings are summarized below:
Coalition hair transplant surgeon Dr. Michael Beehner conducted a comparative study of FUE and FUSS in 4 of his patients. His findings are summarized below:
Objective:
The aim of this study is to see if using FUE for donor harvesting gives the same high yields that have been obtained for years using FUSS with strip harvesting and microscopic dissection of grafts.
Materials and Methods:
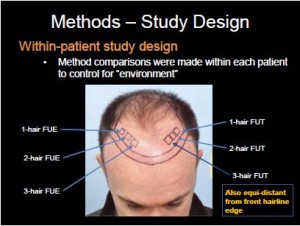
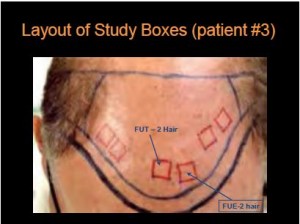
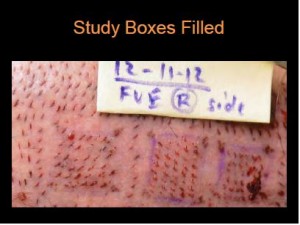
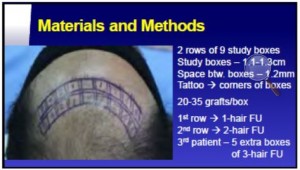
As shown in the image below, patients had six boxes measuring 1.2cm x 1.2cm drawn on to bald scalp. Dots were tattooed in the corners of the boxes and an area of bare scalp 2mm wide was left around each box to minimize confusion in later hair counts.
Recipient site incisions were made using 0.8mm lateral slit blades for the 1-hair follicular unit grafts and 1.0mm blades for the 2-hair and 3-hair grafts.
The first two patients had one box each for 1-hair, 2-hair, and 3-hair grafts using both strip and FUE harvesting methods.
The third patient received 4 study boxes for 2-hair grafts and 2 boxes for 1-hair FU’s. The fourth patient also had 6 boxes studied (3 for each modality) with 4 having all 2-hair grafts and 2 boxes with 3-hair grafts.
The strip was first harvested and then FUE was performed in the region just below or above that sutured line in the occipital region. The Safe-II system was used with both 0.9 and 1.0mm diameter punches. Mild tumescence was used prior to the FUE extraction.
Discussion and results:
The first two patients had hair counts done at 13.5 months and 9.7 months respectively. The last two patients had their transplant procedure and research study performed on 6-3-14 and 7-30-14 respectively.
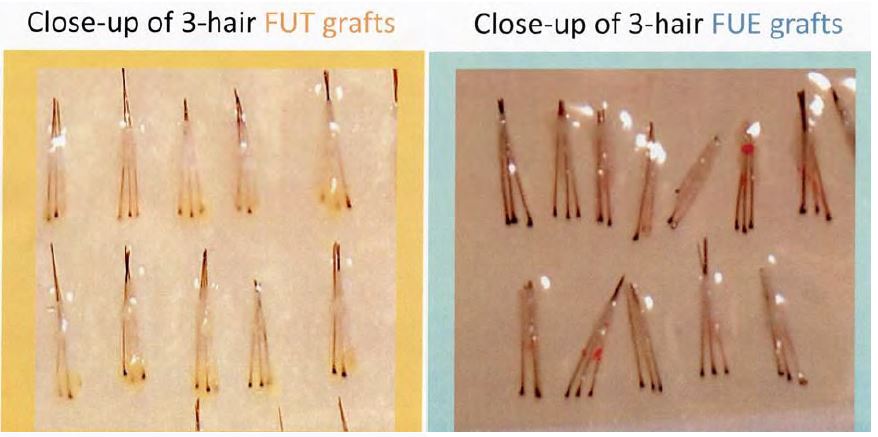
The survival and growth results from the first two patients are shown in the below tables. In all four patients the lower half of the FUE grafts were mostly stripped of fatty tissue and the bulbs were mostly “naked” without protective tissue. This is seen in the two photos of 3-hair grafts from patient #2.
Summary:
Based on this study of 1780 FU grafts in 4 patients, a projection can be made that:
- 11% of all FUT grafts will fail
- 43% of all FUE grafts will fail
At this time, this is the only study of its kind. Thus, other similar studies in the future may show similar or different results
‘Pre-making’ Recipient Sites Before Follicular Unit Harvesting
 Dr. Robert M. Bernstein, an esteemed member of the Coalition of Independent Hair Restoration Physicians, presented a simple modification in the sequence of the major steps in a Follicular Unit Extraction (FUE) hair transplant that will be beneficial to both healing and growth following the procedure.
Dr. Robert M. Bernstein, an esteemed member of the Coalition of Independent Hair Restoration Physicians, presented a simple modification in the sequence of the major steps in a Follicular Unit Extraction (FUE) hair transplant that will be beneficial to both healing and growth following the procedure.
It has been standard operating procedure in FUE to create recipient sites after graft harvesting and then place the grafts into these sites. Dr. Bernstein showed the numerous benefits of reversing the order and making recipient sites before grafts are harvested.
This simple change in procedure shortens the time that grafts are outside of the body and decreases the risk of metabolic injury. By creating recipient sites before harvesting, the sites begin to heal, and so exhibit less bleeding during placement. As a result, fewer grafts “pop” out of the recipient wound and there is less mechanical trauma to grafts because fewer of them need to be re-positioned after popping. Allowing additional healing time for the sites also provides a more fertile bed for the newly implanted follicular unit grafts.
Dr. Bernstein proposed that the surgeon might deliberately delay extraction in some large FUE sessions up to 24 hours. This allows the pre-made recipient sites additional time to heal and creates an optimal environment for the newly transplanted grafts.
In sum, Dr. Bernstein described how a modification of the traditional steps in FUE could impact the outcome of every FUE hair transplant. Given the popularity of FUE hair transplants (now about 50% of all hair transplant procedures), this small procedural adjustment could result in an improved outcome for thousands of patients around the world.
Body Hair Transplant by Follicular Unit Extraction
 Aside from the potential to deliver less visible scarring in the hair transplant donor area, FUE offers surgeons the ability to harvest FU’s from virtually any part of the body including the beard, chest and legs. Recommended hair transplant surgeon Dr. Sanusi Umar is a pioneer in the study and practice of body hair transplants (BHT)
Aside from the potential to deliver less visible scarring in the hair transplant donor area, FUE offers surgeons the ability to harvest FU’s from virtually any part of the body including the beard, chest and legs. Recommended hair transplant surgeon Dr. Sanusi Umar is a pioneer in the study and practice of body hair transplants (BHT)
In the following study, Dr. Umar presents data based on the cases of 124 patients who underwent FUE using customized punches utilizing donor hair derived from non head areas (beard, neck, trunk, limbs, armpits, and pubic hair). All patients were e-mailed surveys from June 2011 through June 2012 to assess their surgical outcomes and overall satisfaction.
Results
Seventy-nine patients (67.5%) responded to the survey. The mean transplanted graft count was 4,308 follicles (standard deviation: 3,577, range: 309-17,183). Patients were generally very satisfied with the results of their procedure, giving mean scores of at least a 7.7 (scale of 0-10) for their healing status, hair growth in the recipient areas, and overall satisfaction with their surgeries. This satisfaction trend was sustained in patients whose donor areas came from outside the head and neck areas.
The mean scores provided by patients with body hair donor sources were comparable to the mean scores provided by patients with SDA sources.
Conclusions
FUE using body hair can be an effective hair transplantation method for a select patient population of hirsute individuals who suffer from severe baldness or have little or no hair in their safe donor area.
FUE, Regrowth Rate of Transected Hair in the Donor Area
 Coalition hair transplant surgeon Dr. Jean Devroye presented the following results if his study on the regrowth rate of transected hair in the hair transplant donor area:
Coalition hair transplant surgeon Dr. Jean Devroye presented the following results if his study on the regrowth rate of transected hair in the hair transplant donor area:
Introduction:
For a few years the ISHRS FUE Research Committee has been working on different subjects and study designs related to FUE. Two years ago Dr. Devroye proposed to study the consequence of the transections in the donor area. This idea came from two observations: one was the observation of a completely devastated donor area on a patient coming back from Turkey where he had a big FUE mega-session of about 7000 grafts in one step. The second was his personal observation of the donor area of his patients and the discussions he had with some other members of the committee.
Dr. Devroye’s clinic had a completely opposite view of the consequences of transections. Dr. Devroye’s opinion was that transections are probably more damaging, and therefore cosmetically significant, than what is generally appreciated, and he has always been a big fan of limiting damage caused by FUE techniques. The opinion of some of his colleagues was that transections were not important because they thought that the follicles were always growing back. Dr. Devroye wanted to know the truth. So, the objective of this study was to know how many follicles are growing back in the donor area after a complete transection and to study the relation between the depth of the transection and the viability of the remaining part of the follicle.
Protocol:
It took a very long time to find a good protocol. Dr. Devroye first tried to study the consequence of transections on some of his routine patients. He finally realized it was almost impossible to approach the matter in this way for two main reasons:
First, the patient has to be evaluated very often and it’s not easy to find a patient available to come back several times for a long-term follow-up. Additionally, he needed to systematically shave the area studied and, again, it’s not easy to find a patient who is willing to go along with this.
Therefore, Dr. Devroye tried to find a protocol as close as possible to his daily practice. He finally opted for a complete transection of the whole follicular unit. The only difference with the everyday reality involving transection is that usually they transect one or two hair follicles, not all the follicles in a given unit.
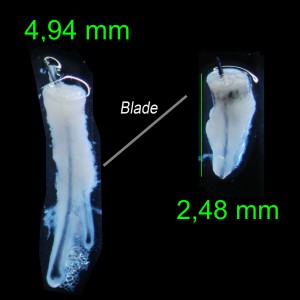
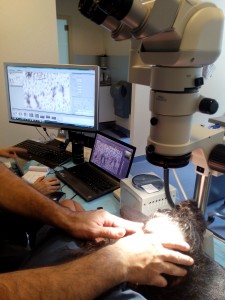
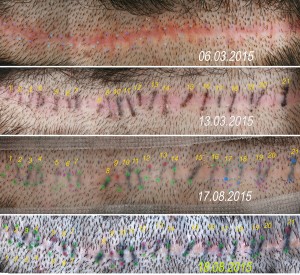
Moreover he had to dissect the FU deep enough (+-3 to 3.5 mm) to poll it and allow him to cut with a little blade the upper part of the follicle at the right place. (fig.1) View of the transaction:
A few months ago, Dr. Devroye had the opportunity to perform a surgery on one of his female technicians. The team placed more than 3000 grafts on the front area and she accepted to be the principal subject for this study.
The result of her hair transplant is stunning and she is very happy with it. (Dr. Devroye would like to thank her for her wonderful devotion and for accepting all these long sequences of observation and shaving yet, unfortunately for her, it’s not finished yet!)
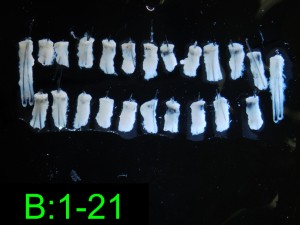
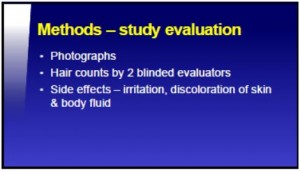
The area studied is around the strip scar. A tattoo improves the localization of the follicles transected. All the hairs of 42 FU were completely transected. Each top part transected was photographed and the level of transection measured and compared with two intact follicles. The area was precisely followed for a 6 month period.
A large number of photographs were required for accurate documentation. In order to have an accurate analysis, Dr. Devroye took pictures with a good flash, increased the depth of field and often blended different pictures with Photoshop to obtain a very detailed view (fig 2) Serial of FU transected:
The size of the final document was 10,000 pixels by 10,000 pixels: 100 million pixels!
Actual counting was made directly by finding and counting each follicular unit transected on the head by examining the scalp under a stereoscope. Dr. Devroye was aided by the simultaneous use of pictures, along with dual screen monitors, yet the process took more than three hours to complete (Fig 3) Counting the grafts with the microscope and screens:
Results of the Observation:
From 42 FU transected, 38 were available for a study, and this amounted to a total of 84 follicles. The reference length of an intact FU was 4,94 mm (Fig.4) Donor area, before and after regrowth:
40% to 70% of the top was removed in each transection.
After 5 ½ months, only 60% of the follicles grew back (Out of 84 total follicles studied, 34 produced no hair) and 8 FU were completely empty. 3 hairs were miniaturized.
Bias, Doubt, Criticism:
Dr. Devroye feels the design allows a very accurate follow- up. But the follow- up has to be at least one year and the recognition of the follicle is so difficult and time consuming, he had to try to improve the protocol.
This kind of study requires good instrumentation. He personally prefers using a Nikon stereoscope with a Nikon camera, and Zeiss Loops numbers 6 and 8. He also used a Canon camera with 100 mm macro and macro device.
Dr. Devroye has already begun another study on the same patient. Two months ago 100 FU were transected for a total of 200 individual hairs. He transected 2 to 4 follicles disposed in one line.
The goal is to facilitate the recognition of the follicles transected; nothing looks more like a follicle than another follicle! His team has again taken some precise pictures of each transected follicle in order to be able to measure the depth of the transection.
Dr. Devroye will have more results and observations to present during the next meeting in Panama.
 What is the Future of Follicular Unit Extraction (FUE)?
What is the Future of Follicular Unit Extraction (FUE)?
Regarding the present and future of FUE, Coalition hair transplant surgeon Dr. Damkerng Pathomvanich contributed the following the summary:
FUE is on the rise and almost catches up with strip. Dr. James Harris summarized that there are two basic punch designs currently in use today to perform FUE: sharp and dull punch. The difference between the two types dictates the dissection technique, the maximum depth to which the punch can be inserted, the force required for extraction and the speed of dissection. Each basic design has inherent advantages and disadvantages.
Dr. David Josephitis of Shapiro Medical Group studied 20 consecutive FUE patients side by side, comparing the use of a 0.9 mm sharp vs dull punch and found very little differences in transection rates and overall yield between the dull and sharp punch. Findings of transection rates of less than 3% and 2.8 hairs per graft were noted in both groups. However, results vary depending on hair characteristic and racial differences.
A combination of FUE and Strip is also on the fast track to gain more grafts and thus minimize wide donor scars from follicular unit strip sugery, at the same time reducing the chances of diffuse donor hair thinning from FUE. However, the combo technique can lead to a wider strip scar.
Innovative and Future Hair Loss Treatments
 Microneedling is the process of passing a tiny roller called a Dermaroller, lined with hundreds of very small needles, over the skin. The benefits of microneedling are said to include; removing wrinkles, fading acne scars and stretch marks, and even inducing hair growth.
Microneedling is the process of passing a tiny roller called a Dermaroller, lined with hundreds of very small needles, over the skin. The benefits of microneedling are said to include; removing wrinkles, fading acne scars and stretch marks, and even inducing hair growth.
In a presentation titled, “Effect of Microneedling in Patients having Androgenic Alopecia”, Dr. Ummer Yaseen of India tested the Dermaroller’s ability to regrow hair.
Background:
Rogaine (minoxidil) and Propecia (finasteride are the only FDA approved treatment options for androgenic alopecia.
Aim:
The aim of our study was to see the result of Dermaroller in androgeneic Alopecia.
Material and methods:
50 patients were selected and divided into two groups. In the first group minoxidil and finasteride were used, in the second minoxidil, finasteride and Dermaroller were used.
Results and conclusions:
Though the presentation does not quote statistics, Dr. Yaseen reports that they observed that hair growth was better in the group that used the Dermaroller combined with minoxidil and finasteride.
Optimal Graft Storage Solutions to Maximize Hair Growth
Holding solutions are used in hair transplantation to store the follicular unit grafts after they are harvested and while awaiting implantation. Graft storage is a crucial aspect of surgery as inappropriate storage can lead to desiccation and poor hair growth.
 In his presentation titled “Update on Holding Solutions”, Dr. Bill Parsley discusses today’s top solutions from simple saline to advanced formulations. Of the numerous solutions available, normal saline remains the most commonly used in spite of many attempts to attract surgeons to some of the more advanced solutions.
In his presentation titled “Update on Holding Solutions”, Dr. Bill Parsley discusses today’s top solutions from simple saline to advanced formulations. Of the numerous solutions available, normal saline remains the most commonly used in spite of many attempts to attract surgeons to some of the more advanced solutions.
According to Dr. Parsley, “Much work and good studies are still needed to guide hair surgeons in their search for the best holding solutions along with deciding which solution is best for different clinical situations.”
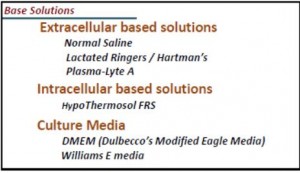
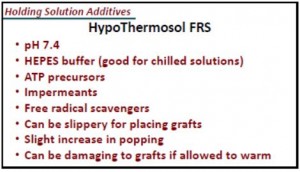
Conclusion:
Hair grafts are tougher than solid organs. Less than optimal hair growth may be improved by a better holding solution. Poor growth is not likely due to the solution.
The greater the Time out of Body, the greater the importance of the holding solution. Keeping grafts wet is of primary importance.
Methylene Blue as a Storage Solution
 Coalition hair transplant surgeon Dr. Damkerng Pathomvanich of Thailand contributed to a study on the efficacy and safety of Methylene Blue as a storage solution in hair transplantation.
Coalition hair transplant surgeon Dr. Damkerng Pathomvanich of Thailand contributed to a study on the efficacy and safety of Methylene Blue as a storage solution in hair transplantation.
Patient population:
Three subjects 18 years of age or older with male pattern hair loss (Norwood-Hamilton class IV-VI) were chosen for this study. Patients were excluded if they (a) had underlying unstable medical conditions, (b) received topical medication for the hair loss within 6 months, (c) took finasteride or dutasteride or oral minoxidil within 12 months, (d) received light or laser therapy for the hair loss within 3 months, (e) received any medications which can cause hypotrichosis or hypertrichosis, (f) received any other treatments which can affect hair growth, or (g) were allergic to MB.
Study design:
This was a pilot study. All subjects gave their informed consent before entering the study. The subjects were required to participate in eight post-surgical evaluations during the course of the study – on the surgery date and seven follow-ups at 1 day, 7 days, 1 month, 4 months, 8 months, 12 months and 18 months.
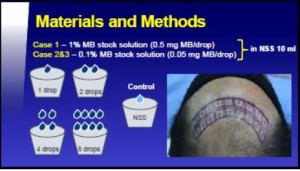
Before surgery, 2 rows of nine study boxes were marked at the end of hair line on top of the forehead (see image below). The corners of each box were tattooed and a 1.2 mm wide bald skin area was left around each box. Boxes were designed for 20-35 grafts per box from four different types of storage solutions. In each row the center box was used for grafts prepared in NSS, while the boxes on either side outward were for grafts prepared in 4 different strengths of MB/NSS in the order of 1, 2, 4 and 8 drops respectively.
Conclusion:
Methylene Blue at specific concentrations appears to increase graft survival for better growth rate in hair transplantation. In this pilot study, it has proven to be both safe and effective as a hair graft storage solution.
Creating the Most Natural Looking Hair Transplant Results
Hairlines and crowns typically receive all the glory when it comes to surgical hair restoration. But, many often overlook the importance of temple points in recreating a youthful and natural appearance. In a presentation titled, “Temples of India”, recommended hair transplant surgeon Dr. Tejinder Bhatti noted the following:
 “We all have oftentimes realized that lack of temple triangles makes the individual look older than his age. This happens even in people with a head full of hair. On the contrary, even a completely bald individual with well-preserved temple points looks the same age as he would if he had a head full of hair. This is the most important advantage of having well placed full temple triangles to frame a face in cases that lack them. A successful modern day hair transplant has to not only grow lush hair on the head but also should make it look aesthetic, youthful and natural which is achieved not only through a soft hairline. Other parameters like a well framed face through temple point reconstruction, etc. underline the signature of the hair restoration surgeon.”
“We all have oftentimes realized that lack of temple triangles makes the individual look older than his age. This happens even in people with a head full of hair. On the contrary, even a completely bald individual with well-preserved temple points looks the same age as he would if he had a head full of hair. This is the most important advantage of having well placed full temple triangles to frame a face in cases that lack them. A successful modern day hair transplant has to not only grow lush hair on the head but also should make it look aesthetic, youthful and natural which is achieved not only through a soft hairline. Other parameters like a well framed face through temple point reconstruction, etc. underline the signature of the hair restoration surgeon.”
Aims and Objectives
Present over 10 cases of temple points and results after one year. The philosophy and technique shall be discussed. Badly placed temple points and how they were revised shall also be discussed with photographic details.
Technique
The points to be kept in mind while reconstructing effaced temple points are:
- Overall facial profile
- Age
- Ethnicity
- Objectives of the patient
- Acceptable surgical norms of temple point reconstruction
- Angle of exit of hair
- Curl of hair shaft
Patient Examples
Updates on Laser Therapy: Is it an Effective Hair Loss Treatment?
Lasers remain an intriguing, yet controversial hair loss treatment. While some of the world’s leading hair restoration experts believe low level laser treatment (LLLT) improve hair growth, other equally reputable physicians refute this.
 According to a presentation by Coalition hair transplant surgeon Dr. Robert Haber, “low level laser therapy is a legitimate therapeutic modality for properly selected patients with hair loss, and should be understood by hair loss experts.”
According to a presentation by Coalition hair transplant surgeon Dr. Robert Haber, “low level laser therapy is a legitimate therapeutic modality for properly selected patients with hair loss, and should be understood by hair loss experts.”
In another study, Dr. Ratchathorn Panchaprateep shared data suggesting that a combination of a non-ablative 1,550 nm erbium: glass fractional laser and mesotherapy using autologous platelet-rich plasma (PRP) is a safe and effective treatment option for both male and female androgenic alopecia.
Materials and Methods:
In Dr. Panchaprateep’s study, six women (Ludwig Scale classification I-III) and three men (Norwood Scale classification IIIv-IV) with genetic hair loss underwent two sessions of non-ablative fractional laser followed by PRP injection on the affected area at 1-month intervals.
Clinical efficacy was analyzed by global photography assessment using standardizing seven-point rating scale (-3 to +3), target area hair counts, hair mass index (Haircheck®) and patient self-assessment. Adverse events were recorded and pain was scored using a visual analog scale (VAS).
Results:
At 6 months after completing the treatment, all patients improved as observed by the global photography of vertex area (two were slightly, three moderately, and four markedly improved) compared to baseline.
Hair density (terminal hair count) significantly increased by 17.8% (105.7±4.5 to 124.6±41/cm2) (p=0.008). Hair mass index also showed significant increase by 17.3% (30.22±9.1 to 35.44±11.9) (p=0.008). The treatment is well-tolerated and the mean VAS for pain was 2.7 (0-5) and 5.8 (3-8) for laser treatment and PRP injection, respectively.
Operation Restore to the Rescue
Operation Restore is a Pro Bono program created by the ISHRS in 2004, that matches prospective patients suffering from hair loss due to trauma or disease with qualified hair restoration surgeons willing to volunteer their surgical services. The program provides financial, travel, lodging, and medical assistance to eligible patients who cannot afford the cost of hair restoration surgery.
This year, the program panel discussion was moderated by Coalition hair transplant surgeon and Operation Restore contributor, Dr. James Vogel. Examples presented included patients with burns, congenital malformations and tumor treatments all resulting in hair loss.
Here, Dr. Vogel (left) poses with with a 3 year old sponsored by Operation Restore who required tissue expanders for reconstruction of a scalp defect following surgery for a brain tumor and radiation and chemotherapy.

The ISHRS is to be commended for many past years of sponsoring this program in which nearly $600,000 dollars of benefits have been provided to deserving individuals with hair loss at no charge to the patient.
Meeting Summary
Medical and surgical hair restoration have continued to grow and advance thanks to the efforts of skilled and experienced hair restoration physicians like those recommended on The Hair Transplant Network.
Our thanks to those physicians who attended this year’s ISHRS meeting in Chicago and contributed to the writing of this presentation.
—-
David
Editorial Assistant and Forum Co-Moderator for the Hair Transplant Network, the Coalition Hair Loss Learning Center, and the Hair Loss Q & A Blog.
To share ideas with other hair loss sufferers visit the hair loss forum and social community.
Technorati Tags: hair restoration, Follicular Unit Extraction, FUE, hair loss treatments, hair transplantation, balding, hair growth, bald, follicular unit, hair transplants, body hair transplants, BHT, Microneedling, Dermaroller, hair growth, Androgenic Alopecia, regrow hair, Rogaine, minoxidil, Propecia, finasteride, low level laser treatment, LLLT, platelet-rich plasma, PRP, female androgenic alopecia, Ludwig Scale, Norwood Scale